A New Method for the Development of Escherichia Coli Resisitant Against Antibiotic Ampicillin
Bacteria are like living paint, covering nearly every surface imaginable and living within a variety of living and nonliving things. An antibiotic is any substance produced by a microorganism, which harms or kills another microorganism. However, antibiotics do not harm viruses. A majority of antibiotic substances are natural products that certain bacteria and fungi produce as a natural defense to send outside their cells.
The whole 9 pages article is available for download here.
Ampicillin is a prescription drug, introduced in 1961, used to treat infections caused by certain bacteria, including the specific bacteria family Enterobacteriaceae. Ampicillin is an antibiotic (drug produced by microbes). It is a semi-synthetic form of penicillin, belonging to the penicillin group of drugs. The present work was conceived to determine if Escherichia coli has the ability to become resistant to the antibiotic ampicillin and if yes, conclude the amount of time involved and how effective the mutant ability is.
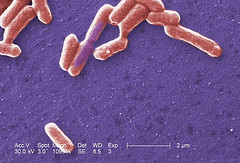
E. coli, the most significant species in the genus Escherichia, is recognized as an important potential pathogen in humans. Being a gram-negative bacillus, it is a common isolate from the colon flora. E. coli are found in every human being's intestines. E. coli are essential for producing the particular vitamins K and B-complex. Our bodies are dependent on E. coli for the production of these vitamins, our only source. Although we are dependent on these helpful strains of E. coli there are some harmful strains of E. coli (like the O157:H7 strain of E. coli) that have been associated with a wide variety of diseases and infections, including meningeal (predominantly in the newborn), gastrointestinal, urinary tract, wound, and bacteremic infections in all age groups.. The prescription antibiotic ampicillin is a semi-synthetic form of penicillin. Ampicillin is also proven effective against the bacteria family Enterobacteriaceae. On most occasions it may become visible as a non-lactose-fermenter or as a mucoid colony, E. coli usually produces a dry, pink (lactose positive) colony with a surrounding pink area of precipitated bile salts on Mac Conkey agar. The E. coli organism also possesses O, H, and K antigens. E. coli, first described by Theodore Esherich in 1885 was considered a non-harmful member of the colon flora. Since then, E. coli has been associated with a wide variety of diseases and infections, including meningeal (predominantly in the newborn), gastrointestinal, urinary tract, wound, and bacteremic infections in all age groups. E. coli may cause numerous types of diarrheal illnesses. There are five major categories of diarrheogenic E. coli. These include Enteropathogenic (EPEC), Enterotoxigenic (ETEC), Enteroinvasive (EIEC), Enterohemorrhagic (EHEC serotype O157:H7) and Enteroadherent (EAEC).
About 90% of antibiotics used today come from bacteria. Although these are all natural, some antibiotics are completely synthetic (made in a laboratory) and some are semi-synthetic (only altered). To determine which antibiotic works best against a specific bacterium, tests are done in laboratories, such as a susceptibility test. On an agar plate a bacterium suspension is spread over the plate. Then small, circular, sterile disks, saturated with an antibiotic are placed on the bacterium covered agar plate. The plate is then incubated. After incubation the zone sizes around each disk are recorded for resistance or not. Where no growth occurred around disk, the bacterium is sensitive. Where growth around the disk occurs, the bacterium is resistant to that certain antibiotic. One of the major problems we face today is that many of the disease-causing bacteria have become resistant to the effects of different antibiotics. This occurs when a (need only be one cell) bacteria population genetically acquires the ability to destroy the antibiotic. This one resistant cell will divide and produce a population that is now no longer harmed by that particular antibiotic. This is a great concern, because certain strains of disease-causing bacteria now have only one antibiotic remaining which will kill them. Due to this concern there are tremendous efforts in finding new natural sources of antibiotics, and or make completely synthetic ones in the laboratory. One of the reasons for the cause of this problem is because of prior, indiscriminate use of antibiotics in human and domestic animal health (usually cattle and pigs).
The whole 9 pages article is available for download here.